Mahasweta Pal, freelance medical writer at Kolabtree, writes about ongoing clinical trials to test the efficacy of convalescent plasma treatment for COVID-19.
To date, Remdesivir and Favipiravir remain the only available medications with an emergency FDA-approved status to treat coronavirus disease, which are approved and accessible only in a few countries (United States, Italy, China, and Japan). Moreover, hydroxychloroquine and chloroquine, which were the most frequently used medications against SARS-COV-2 infections, have been associated with severe heart rhythm problems and another fresh study concluded that although they are effective against autoimmune disease and malaria, they could not show any significant amelioratory benefit against coronavirus infection. Even the World Health Organization’s SOLIDARITY trial arm based on hydroxychloroquine was halted.
In several countries, the patient population comprises asymptomatic COVID-19 cases, and the need for treatments against mild and severe cases of COVID-19 has risen considerably, which has led to pharma majors considering other treatments under clinical testing, given the emergent global crisis.
Previous studies on treating coronavirus infections such as SARS, MERS, and other viral diseases including the Ebolavirus and H1N1 influenza A pandemics have shown that convalescent plasma infusion is a viable interim solution for treating patients with life-threatening manifestations of severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) coronavirus disease. Therefore, here is a brief look at how this biological intervention is helping in the pandemic management in healthcare systems worldwide.
Clinical Trials on Convalescent Plasma Therapy
In the 96 trials running globally, convalescent plasma (CP) containing antibodies to SARS-CoV-2 is being studied as an investigational treatment for patients with COVID-19. Treatment with CP or hyperimmune immunoglobulin has been restricted to single-arm designs mostly. Until now, 56200+ patients have been recruited into trials while recruitment remains open in most centers. The most common outcome measure in each trial is the change in Sequential Organ Failure Assessment (SOFA) scores measured 1, 3, 7, and 28 days after CP administration on Day 0 of the trial. The inclusion criteria for CP trials are adult severely ill patients, patients with moderately severe complications including respiratory and/or multisystem failure, and patients with a moderate clinical presentation but with long-term comorbidities including diabetes, hypertension, or rheumatoid conditions.
A critical study involving 10 severely ill COVID-19 patients from 3 different hospitals in Wuhan suggested that high-titer CP transfusion can effectively neutralize SARS-CoV-2, leading to impeded inflammatory responses and improved symptom conditions without severe adverse events.
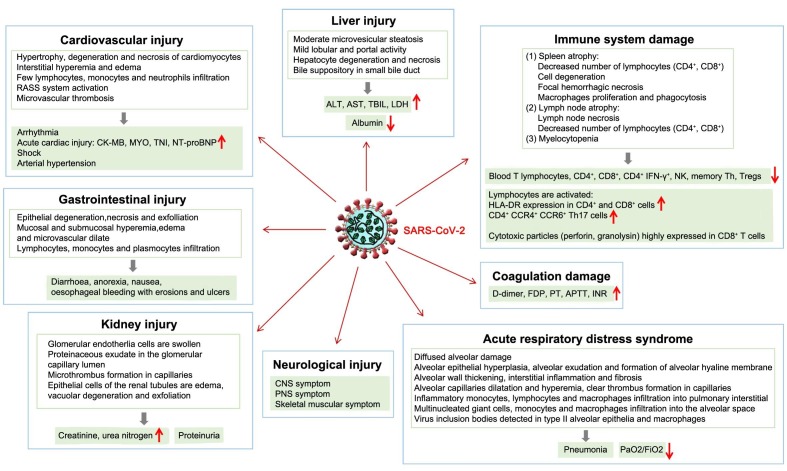
Early Phase I studies conducted in various hospitals across China concluded that CP administration improved respiratory symptoms in 3-5 days after transfusion. In another study, patients had improved SOFA scores and reduced viral load after receiving CP combined with methylprednisolone, mechanical ventilation, and antiviral agents. The treatment was able to provide recovery from ARDS within 12 days, thus showing the applicability of CP in a cohort of small critically ill patients with COVID-19 and ARDS.
One ongoing trial in Colombia is testing the efficacy of Convalescent plasma with Hydroxychloroquine versus Hydroxychloroquine on hospitalized COVID-19 patients. The investigators are looking to evaluate the changes in Viral Load over 1-, 4-, 7-, 14-, and 28-day periods, and IgM and IgG antibody development as primary outcome measures and reduction of hospitalization period and ICU admission as the secondary outcome measure. The NIH has also initiated a clinical trial to collect plasma from adult patients who have recovered from the disease. Interested plasma donors can also look at this nationwide resource by the NIH and US Public Health and pandemic response team dedicated to medical centers enabling safe plasma collection.
USFDA’s Directive on Investigational Clinical Use of Convalescent Plasma
The treatment is to be administered only as an emergency intervention through clinical trials, Expanded Access IND Applications (the provision by the FDA for patients who could not be included in clinical trials), and Single Patient Emergency IND (COVID-19 patients excluded from trials but in serious life-threatening conditions) requested by the chief physicians of the hospital or medical center.
The USFDA is stringent with the administration of CP because these clinical studies pose the risk of exposing patients to potentially immunogenic antigens that will complicate future transfusions, and it will put patients at risk for transfusion reactions. Furthermore, the use of standard plasma as the control arm, which carries many of the same risks of CP but none of its benefits, may mask some of the risks of using CP that could be detected otherwise.
Mechanism of Convalescent Plasma Infusion Therapy
Convalescent blood components are derived from the serum or whole blood of patients who showed recovery from the specific infection (in this case COVID-19) and are considered as the source of SARS-CoV-2-neutralizing antibodies. Historically, passive immune therapy has involved convalescent whole blood, convalescent plasma, pooled human immunoglobulin for intravenous or intramuscular administration, high-titer human immunoglobulin, and polyclonal or monoclonal antibodies. However, plasma collected by apheresis is currently the preferred therapy. Convalescent blood products have a long track record of safety; however, they can increase the risk of antibody dependant enhancement of infection (ADE), a phenomenon that can make a person susceptible to infection with other viruses in the presence of antibodies.
Despite the longstanding evidence of the usage of CP or hyperimmune immunoglobulin, its clinical efficacy remains unclear with weak conclusions, likely because CP was used only in critical situations, during massive epidemic/pandemic outbreaks, requiring immediate actions. The effectiveness of CP therapy appears to differ depending on the pathogen and treatment protocols (eg, timing, volume, and dosing of administration).
Since this is one of the few available viable treatments under application against the 2019-nCoV, there is an impending need for governments to formulate healthcare practice guidelines. Guidelines that ensure biosafety of collected medicinal and biological products, their storage and overall safety, and preventing contamination have yet to be set in place. A key commentary by USFDA in collaboration with researchers from other key COVID-19 institutions also highlights the need for low and middle-income countries to ensure that an adequate supply of quality and safe blood components should be maintained for transfusion, which is essential to meet the primary healthcare needs of the population. The COVID-19 epidemic responses reinstate the importance of building an organized and sustainable national blood system whilst steps are taken to provide appropriately collected, tested, and processed COVID-19 convalescent plasma for investigational clinical use.
Convalescent plasma’s immediate use enables a promising method of managing COVID-19 patients while specific vaccines and treatments are evaluated and brought to scale. CP from donors who recovered from COVID-19 is considered as the most promising when used as prophylaxis or when administered shortly after symptom onset (within 14 days). The immunity is considered to last from weeks to months.